Dysautonomia refers to a range of disorders that affect the autonomic nervous system (ANS), which controls essential bodily functions like heart rate, blood pressure, digestion, and temperature regulation. When the ANS is disrupted, it can cause a variety of symptoms that interfere with daily life. Although dysautonomia can result from many different underlying conditions, it’s increasingly being linked to head injuries, including concussions. In this blog, we’ll examine the different types of dysautonomia, how head trauma can trigger these conditions, common symptoms to watch for, and how functional neurology can support recovery and symptom management.
Types of Dysautonomia
Dysautonomia refers to a group of conditions that affect the autonomic nervous system—the part of the body that controls involuntary functions such as heart rate, blood pressure, digestion, and temperature regulation. Below are some common forms:
-
Postural Orthostatic Tachycardia Syndrome (POTS):
This condition involves a significant increase in heart rate when standing up, often leading to symptoms like dizziness, fatigue, brain fog, and heart palpitations. -
Neurocardiogenic Syncope (NCS):
Also known as vasovagal syncope, this form causes fainting due to a sudden drop in blood pressure and heart rate. It’s commonly triggered by stress, pain, or standing for long periods. -
Orthostatic Intolerance (OI):
Refers to difficulty regulating blood pressure and circulation when standing, which can cause symptoms like dizziness, weakness, and trouble concentrating. -
Orthostatic Hypotension:
This is a drop in blood pressure when standing up, which can cause lightheadedness, blurred vision, fainting, and reduced blood flow to the brain. -
Post-Concussion Autonomic Dysfunction:
Some people develop autonomic symptoms after a concussion or head injury, including dizziness, poor tolerance to exercise, sensitivity to temperature, and irregular heart rate.
Please Note:
These are just a few examples of conditions classified under the dysautonomia umbrella—there are approximately 15 recognized types. Some forms may be linked to infections, autoimmune disorders, or neurodegenerative diseases. If you're experiencing symptoms and would like to know if we address your condition, feel free to reach out to our office.
Dysautonomia and Head Injury
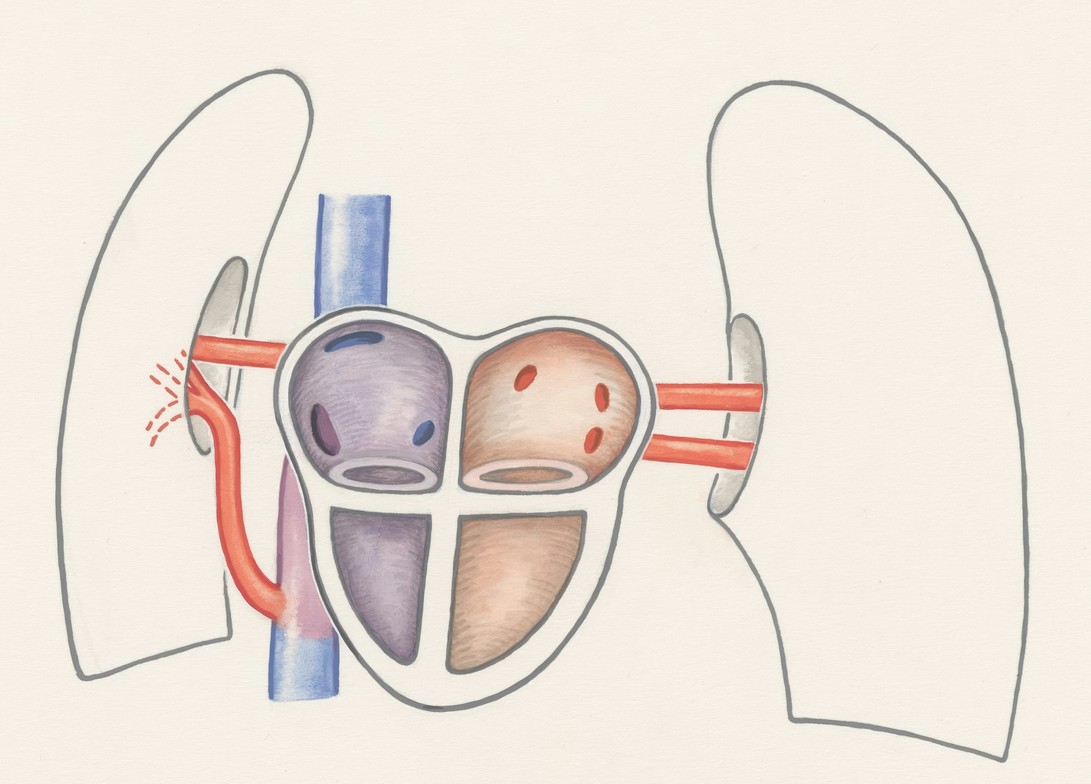
Head injuries, including concussions and traumatic brain injuries (TBI), can interfere with autonomic nervous system function by impacting key areas of the brain such as the brainstem, cerebellum, and limbic system. These regions play a crucial role in regulating communication between the brain and body. When disrupted, this communication breakdown can lead to a variety of symptoms, including:
-
Dizziness or lightheadedness, especially when standing up quickly
-
Rapid heart rate (tachycardia) or low blood pressure
-
Difficulty tolerating physical activity (exercise intolerance)
-
Problems with temperature regulation
-
Mental fog, poor focus, or trouble concentrating
-
Gastrointestinal issues such as nausea, bloating, or irregular digestion
-
Persistent fatigue and reduced ability to handle stress
-
Pressure headaches
These symptoms can significantly affect quality of life and may persist long after the initial injury.
How Functional Neurology Supports Recovery from Dysautonomia
Functional neurology takes a personalized approach to dysautonomia by addressing the root cause—neurological dysfunction—rather than simply managing symptoms. This method is especially effective for individuals whose dysautonomia began or worsened after a head injury.
Core Treatment Strategies:
Neurological Rehabilitation
Customized brain-based exercises help improve the function of the brainstem and cerebellum, leading to better autonomic regulation and nervous system stability.
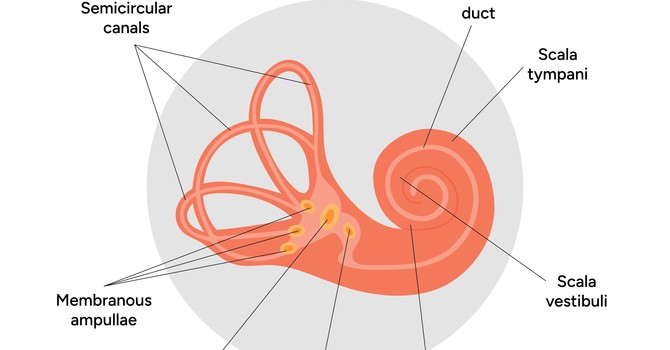
Vestibular and Oculomotor Therapy
These therapies restore balance, visual tracking, and spatial orientation—essential for preventing dizziness and instability. Head injuries often disrupt the brain’s ability to interpret signals about body position and movement. If your brain can't accurately sense whether you're standing, lying down, or moving, it can’t properly direct blood flow—contributing to dysautonomia symptoms.
Cardiovascular Conditioning
Individually tailored, progressive exercise programs help retrain the body's ability to regulate blood pressure and circulation, improving autonomic flexibility.
Diet and Lifestyle Adjustments
Addressing inflammation, nutritional deficiencies, and hydration can significantly support brain and nervous system health.
Breathwork and Biofeedback
These tools help regulate heart rate variability, reduce stress responses, and build greater resilience within the autonomic nervous system.
A Patient-Focused, Integrative Approach
As a board-certified chiropractic neurologist, my goal is to identify and treat the underlying neurological factors driving dysautonomia. By combining advanced neurological and vestibular rehabilitation with musculoskeletal care and functional medicine, we create customized treatment plans that promote real, lasting improvements in daily function and quality of life.
If you or someone you care about is dealing with dysautonomia—especially after a concussion or traumatic brain injury—functional neurology could be the missing link in your recovery. Reach out to our clinic to learn how we can help.
Forrest Fisher
Contact Me